04 Oct Six Building Blocks for opioid management in chronic pain
Prescription opioid use and misuse have reached a crisis level in the U.S., with roughly 58 opioid prescriptions for every 100 residents in 2017 and more than 46 people dying daily from overdoses involving prescription opioids. (Source: Centers for Disease Control Opioid Prescribing Rate Maps). Although treatment plans and improved support options for managing opioid medications for individuals with chronic pain are being developed, implementing these evidence-based strategies in real world primary care settings can be challenging. Community and healthcare centers that treat patients who use opioids long-term for their chronic pain struggle with this issue and need tools and structured guidance in order to make meaningful change.
Opioid use disorder (sometimes known as addiction) can be a result of the use of opioid medications to treat patients with chronic pain. “We’ve dug a deep hole for ourselves in primary care and in medicine due to the overuse and over prescribing of opioid medications,” described Michael Parchman, MD, MPH, expert in chronic illness care research.

Michael Parchman, MD, MPH
Understanding the landscape
Dr. Parchman, a Senior Investigator at Kaiser Permanente Washington Research Institute, an ITHS collaborating institute, participated in a project funded by the Robert Wood Johnson Foundation: “Primary Care Teams: Learning from Exemplar Ambulatory Practices (LEAP).” The LEAP team identified and visited 30 medical practices across the U.S. that were exemplar models of team-based primary care.
Although not a specific focus of the project, the LEAP team recognized early on that most of these practices had systems in place to manage how opioids were used to treat their patients with chronic pain. “These clinics taught us a lot about how you do this kind of work,” reiterated Dr. Parchman. The results were consistent: the most successful clinics had six common themes, synthesized into “Six Building Blocks” for improving opioid medication management.
In the next step of this endeavor, Dr. Parchman partnered with Laura-Mae Baldwin, MD, MPH on a grant from the Agency for Healthcare Research and Quality (AHRQ) to use the lessons learned from the successful clinics and repurpose them to drive change in clinics struggling to effectively manage their chronic pain patients who use opioids long-term. What resulted was the Six Building Blocks change package, which combines tools and mentored guidance for implementation in clinical practice.
Dr. Baldwin has worked with ITHS to strengthen research and community partnerships across Washington, Wyoming, Alaska, Montana, and Idaho (the WWAMI region). She was instrumental in establishing a network of clinics called the WPRN (WWAMI region Practice and Research Network) that aims to partner with researchers on projects of importance to the communities they serve.

Laura-Mae Baldwin, MD, MPH
The Six Building Blocks project was an ideal candidate for the WPRN. The Agency for Healthcare Research and Quality (AHRQ) grant allowed Drs. Parchman and Baldwin to bring the Six Building Blocks to 20 rural clinics using a facilitated implementation process that provided customized tools, mentored guidance, and shared learning experiences.
What are the Six Building Blocks?
The Six Building Blocks is a team-based intervention for improving opioid prescribing and management.
The Six Building Blocks include:
- Providing leadership support
- Revising and aligning policies, patient agreements, and workflows
- Tracking the patient population
- Offering planned, patient-centered visits
- Identifying resources for complex patients
- Measuring success
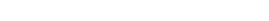
Drs. Baldwin and Parchman worked with their research team, including a practice coach, Brooke Ike MPH, to provide 15 months of external support to implement these six elements in the 20 rural and rural serving clinics within six organizations. “We were coaching them to adopt new ways of managing opioid medications,” said Dr. Baldwin.
Each site first established its own opioid improvement team. The research team held an in-person kickoff meeting with the clinicians, leadership, and other health care providers at each site to conduct an initial self-assessment of their opioid management. Coaches provided materials relating to the Six Building Blocks along with tools for supporting their implementation. Additionally, the study provided an infrastructure for sites to share their experiences by discussing progress, challenges, and working solutions with each other.
AHRQ has promoted and published the Six Building Blocks website to support hands-on coaching and broader dissemination of this program. Learn more about the Six Building Blocks and how they can be used at your organization directly from the resulting website: ImprovingOpioidCare.org
Excerpt from the Implementation Guide.
Spreading impactful results
ITHS is in a unique position to catalyze work that emanates from clinical practices facing a challenging issue such as management of opioid medications for treatment of chronic pain and opioid use disorder. According to Dr. Baldwin, the Six Building Blocks is a “truly community engaged project.” The Six Building blocks were developed in collaboration with community practices, then tested and refined in new practices, and now are available to a broader community.
This is a truly community engaged project
Over the course of the project, the research team saw a significant decline at the study sites in both the percent of patients using high dose opioids and the overall number of patients using opioids for chronic pain. In addition, it was not uncommon for physicians and staff in the clinics to report that patients described how their pain had decreased as they lowered their opioid dose.
“In addition to seeing these numbers improve, we observed that the providers and staff were better able to care for these patients with less stress and burn-out,” said Dr. Baldwin. This particular intervention targeted the practices and health care professionals themselves. Drs. Parchman and Baldwin wanted to see high level changes within an organization, a collaborative team effort in developing a new plan for managing opioids, and more consistency among clinics and between providers. Both qualitative and quantitative data from their study have demonstrated the Six Building Blocks program’s success in shifting clinic culture to reach these goals.
One of the clinics involved in this study won a statewide award for healthcare excellence: Clearwater Valley Hospital and Clinics was one of four recipients of Qualis Health’s 2018 Idaho Award of Excellence in Healthcare Quality as a direct result of this project.

“We could not have done this work without the ITHS infrastructure” emphasized Dr. Parchman, referring to the existing WPRN network and an electronic data sharing tool supported by ITHS called DataQUEST, which allowed the team to easily measure changes in outcome metrics of success.
Where will this project go next?
The Six Building Blocks team has received funding from a multitude of sources so that team members can continue their work at the state and national level.
- The Washington State Department of Health has contracted with the research team to support implementation of the Six Building Blocks program across the state.
- The team is working with the Olympic Communities of Health, one of Washington State’s Accountable Communities of Health to support use of Six Building Blocks within their health care organizations across the three counties covering a large geographic area including the Olympic Peninsula.
- The Centers for Disease Control has incorporated the Six Building Blocks into the implementation strategy within their guidelines for prescribing opioids for chronic pain.
The Six Building Blocks dissemination plan covers hundreds of primary care practices with a catchment area of thousands of patients. Furthermore, AHRQ is providing funding to migrate the existing coached Six Building Blocks toolkit and resources into a more self-sufficient, ‘do-it yourself’ independent change package. The Six Building Blocks team is likely to have a strong role in the development of this new toolkit.
“This is an amazing piece of work” said Dr. Baldwin, highlighting how the team continues to make a difference and “gain traction with a myriad of organizations.”
Learn more
- About the Six Building Blocks: learn about the building blocks and how to use them
- Read the LEAP paper: Primary Care Teams: Learning from Exemplar Ambulatory Practices (LEAP)
- In other news: the AHRQ issued a press release about the six building blocks
This research was funded in part by the Agency for Health Care Research and Quality under grant number R18HS023750.