30 May Pilot Grant Helps Lymphoma Lab Refine Newest Idea

The life of a researcher includes many promising paths that have twists and turns. Oliver Press, MD, PhD, has spent more than 20 years exploring the oncology of blood cancers. He has multiple awards already for progress he has made in treatment of patients with lymphomas, one of several blood cancers. But even an experienced researcher can find himself needing a $50,000 pilot from the ITHS. That was the situation in 2010, when Press and his lab at Fred Hutch were in an awkward stage. They had made progress with a five-year grant from the National Institutes of Health, but THE FIVE YEARS HAD ENDED. The grant’s renewal hung in a sort of limbo. In the meantime, their latest ideas for progress in lymphoma required creating a new compound in the lab.
A pilot from ITHS gave them $50,000, which they used to carefully construct a compound to help treat lymphoma using what is called pretargeted radioimmunotherapy. They later tested this approach in a few lymphoma patients to demonstrate the promise of this strategy. This significant advance led to the renewal of a 5-year NIH grant for about $16 million.
The pilot “allowed us to get the data we needed” for the renewal, Press explained.
Even more significant, perhaps, the promising avenue explored via the pilot led the researchers to explore a similar model for myeloma, another blood cancer. They were awarded two grants for pursuing what is called pre-targeted radioimmunotherapy in regard to myeloma – one for $1.16 million and another for $785,000 (primarily for staff salaries.)
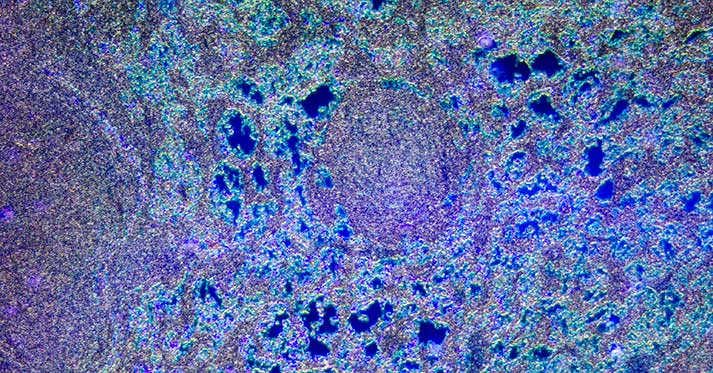
Traditional radioimmunotherapy means that doctors tie together radiation and antibody-specific compounds, so that the radiation is carried directly to tumor cells. Sometimes this is called “targeted” therapy. The tumor cells have a receptor for that antibody on their outside cell wall. Because the two fit together like a lock and key – the radiation is delivered directly to tumor cells and not to healthy tissue. There is a delay of 24 hours or so while the patient’s body responds to the compound, and during that time tissues other than the tumor can be exposed to circulating radiation.
In the new method, which was part of the pilot grant, the patient is given one compound without radiation to prepare them for the subsequent radioimmunotherapy. Within minutes, typically, this second dose reaches the tumor targets while exposing fewer tissues to radiation.
Press is a member of Fred Hutch, a professor in the University of Washington Medical School and a national leader in blood cancer research. He explains the need for translational focus this way:
“Basic science is important for quantum leaps forward in understanding. But once you make those leaps you need to prove that the theories actually work.” ITHS helped his laboratory across a chasm in financing, and kept their work moving forward.
Among his many honors, Press was elected by his peers across the nation to serve as co-chairman of the National Cancer Institute’s Lymphoma Steering Committee, a group that establishes lymphoma research priorities for the United States.
Lymphoma is one of the most common causes of death from cancer in the United States, and about 79,190 new cases of lymphoma are diagnosed every year. In lymphoma, cancer cells are found in the lymphatic system, which is comprised of the bone marrow, lymph nodes, spleen, stomach, intestines and skin.
Combining lab research and patient care works for Press. ” I follow many patients in my clinic who were given our research treatments after standard therapies failed and they were out of conventional options. and Many of these patients have now been in remission for many years following treatment on the research trials. It’s so gratifying.”
For deeper scientific details of this research, see these journal articles:
From the journal, Blood:
- May, 2009 – Comparison of pre-targeting with other radioimmunotherapy.
- July 2011 – High remission in mouse model with pre-targeted radioimmunotherapy.
The project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1RR025014. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.