28 Nov Catching a moving target: motion correction for fetal MRI
Snapping the perfect picture is hard enough when the subject is staying still. Imagine trying to capture a detailed image of an object that is constantly moving at unpredictable velocities. This is precisely the problem that Dr. Colin Studholme, Professor of Pediatrics and Bioengineering, and Adjunct Professor of Radiology, aims to solve by applying his motion correction software to fetal brain imaging. Detailed images of the brain help researchers determine the relationship between brain structure and function. One method to obtain these type of images is through magnetic resonance imaging (MRI). However, in order to obtain an MRI, a person must stay very still in a large, noisy machine. This is not something you can ask of an unborn child. In order to get high quality images of a growing baby, Dr. Studholme and his team have developed a mathematical model and computational technique which uses information from multiple individual MRI images to build a three dimensional map of the baby’s brain.
Earlier in his career, Dr. Studholme began studying images of premature babies. He observed the standard processes for clinical imaging and the challenges clinicians were facing. Blurry images due to movement make it harder for doctors to understand what is going on inside the baby’s head and diagnose a condition. That is when Studholme realized that there could be a way to correct the motion to get a crisper, and more detailed image.

Colin Studholme, PhD
He would also apply a technique called “diffusion imaging” which essentially makes the image sensitive to the motion of water in cells. Typically, MRI is a large pixel image, but when applying diffusion data, one can gather indirect data about the cellular structures within the MRI image. “Essentially, you are using the low resolution imaging to infer the microstructural properties of the tissue.” With this improved technology, Dr. Studholme and his team can observe the connectivity of the brain and integrity of the tissue to see if the microstructures are developing correctly.
With a background in radiology, Dr. Studholme had little experience in clinical trials before this study. In his previous research endeavors, Dr. Studholme received and analyzed data directly from the clinic. This posed a challenge, however, because he only had the resources that were delivered to him. The data and images were not obtained in response to any specific research questions so there was a lot of variation and gaps in the information needed to look at the problems Dr. Studholme wanted to solve. So he began designing his own research project so that he could specifically recruit a cohort of healthy volunteers, take the pictures in a way that yielded the best information, and collect enough data to advance understanding within the field of fetal brain development.
I had not done any of this before, and I could not have done it without ITHS
As a new investigator putting together his first clinical trial, ITHS provided essential experience and support. “I had not done any of this before” Studholme pointed out, “and I could not have done it without ITHS.” The ITHS Research Coordination Center (RCC) provides investigators with a dedicated and experienced coordinator to support research activities for clinical trials.
Before working with the RCC, there had been very little recruitment activity. Dr. Studholme was focused on the protocol and gaining MRI machine access. Research coordinator Jason Caucutt joined the team from the ITHS RCC in order to analyze the study goals and maximize recruitment efforts. ITHS provides tools and resources for research coordinators to maximize recruitment efforts through tried and tested methods. For a more in depth consultation, ITHS also offers Recruitment Support Services tailored to individual study questions and recruitment challenges. After suggesting a few strategy modifications such as a well-placed flyer in the clinic, or IRB approved emails to community LISTSERVs, the study team was averaging four healthy fetus scans per month. This continued to grow to about three scans per week (12 scans per month).
Caucutt also improved recruitment for the more challenging portion of the study: abnormal fetus scans. Previously, the study team had relied on voluntary clinical referrals. Caucutt worked diligently to build relationships with the clinic staff and ensure the study was regularly on their radar. This increased the volume of potential participants. “Each year those numbers just continued to improve: more repeat scans, more word of mouth referrals, and more clinician buy-in bringing us abnormal referrals,” said Caucutt of his most successful efforts. Having a dedicated recruitment specialist allows for the consideration of the full research environment, such as the logistical experience for the participant. In this study, a less hectic clinic with easier parking and an MRI technician who enjoys research provided a pleasant and relaxed experience for potential volunteers which increased participation. To date, the study team has successfully completed 214 scans of normally developing babies, and 32 scans in the abnormal category.
Once the images are captured, how does the motion correction work?
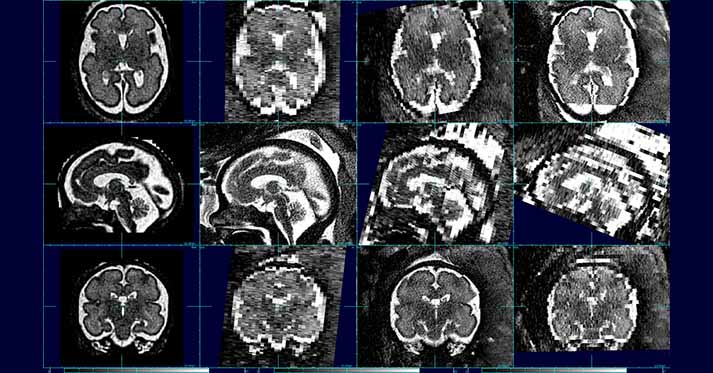
MRI takes a large quantity of very quick two dimensional image ‘slices.’ When the slices are stacked together, one can estimate the full shape and properties of the brain.
The program uses a reference mask to isolate the head from other parts of the body. The first step is stacking the slices properly to estimate how they relate to each other. When looking at these slices over time, the software program creates a model of the movement of the baby’s head while imaging was taking place. This model accounts for many variables, including the time between slices, the directional trajectory of the movement itself, and how the mother’s movement (such as breathing) effects the baby.
With the 214 healthy fetal brain scans, Dr. Studholme has begun to build a library of fetal brain images of varying ages. This technology enables a closer look at the microstructure of the brain which can lead to better questions about the relationship between structure and function. The volume of images also helps define normal variability. With a larger database of fetal images, healthcare professionals can better ascertain where an individual fetus’ development falls compared to other normally developing children and whether or not a brain is trending towards abnormal. Atypical developmental conditions can also be compared.
We are essentially building an atlas of what a brain looks like at whatever gestational age
Says Studholme, which provides clinicians with a “map” to see precisely how an abnormal brain differs from the average and what that could mean for the child’s development. With more data available, the team hopes to discover other associations between structure and function through detailed observation. There is a second phase of this study in which a parent can bring their child into the University of Washington Center on Human Development and Disability for a visit with a child psychologist once they reach 20 months old. This data aims to improve understanding of the connections between behavioral assessments and the visual brain structure. Having that kind of data can help clinicians diagnose early developmental conditions and better understand the important milestones of fetal brain development.
One condition that Dr. Studholme is looking closely at is ventriculomegaly, a situation in which the fluid in the brain leads to oversized ventricles (brain cavities) within the tissue. Typically, ventriculomegaly is diagnosed in a prenatal ultrasound and watched closely thereafter to determine if the baby is developing any further complications due to this condition. Studholme’s technique would provide doctors more detailed, three dimensional images of the brain throughout fetal development.
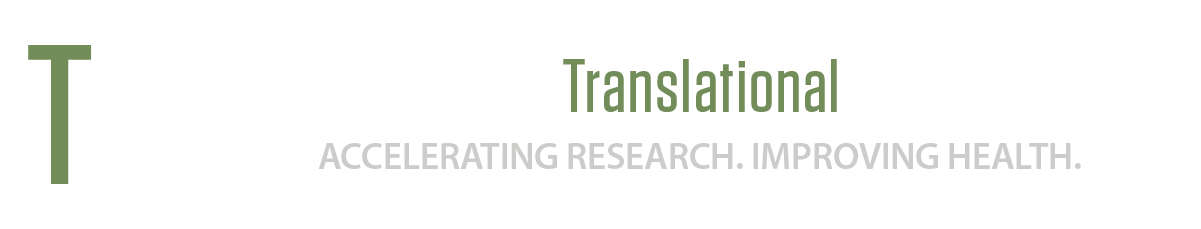
In this image, the detailed MRI allows for a diagnosis of Agenesis of the Corpus Collosum, a condition in which the part of the brain that connects the two hemispheres is missing or incomplete due to a developmental defect. The left part of the image shows each MRI slice placed in context and the right side shows the 3D reconstruction Dr. Studholme and his team were able to obtain with their motion correction technology.
Typically, research in fetal brain development has been limited to imaging lots of babies and hoping to find one that did not move. This process is expensive, time consuming, and dependent on luck. Dr. Studholme’s motion correction technology makes imaging more practical, offering clinicians one more tool to understand, diagnose, and improve the lives of their patients.
Interested in learning more or participating in this study?
Dr. Studholme and his team are still looking for volunteers! If you, or someone you know may be interested in participating, more information can be found on ParticipateInResearch.org. Visit ParticipateInResearch.org